Premature atrial contraction (premature atrial beat / complex)
It is caused by an impulse discharged from an ectopic focus which may be located anywhere in the atria. In most cases, the premature atrial impulse is conducted to the ventricles, which results in ventricular depolarization and the appearance of a QRS complex. Because the impulse originates in the atria it will pass through the bundle of His and thereby produce a normal QRS complex (provided that intraventricular conduction is normal).
A premature atrial contraction induces a delay to the next sinus beat (the RR interval is prolonged after a premature beat). This yields more time to fill the ventricles with blood (increased ventricular filling). Persons with premature beats might perceive this as palpitations, because of the stronger ventricular contractions caused by the increased filling. Frequent premature beats can also be perceived as having an irregular heart rhythm (despite the underlying sinus rhythm).
Although atrial premature beats are virtually harmless, they can trigger sustained supraventricular tachyarrhythmias (e.g. atrial fibrillation, AVNRT, AVRT, etc). This will be discussed later.
Premature atrial contraction on ECG
A premature atrial contraction occurs when an ectopic focus in the atria discharges before the next sinus impulse. The premature impulse may depolarize the atria and subsequently, the ventricles, provided that the myocardium and conduction system have repolarized. This appears as a P-wave and QRS complex occurring earlier than expected (Figure 1). The interval from the premature beat to the next sinus beat will be longer than one normal sinus interval.
The P-wave of a premature atrial contraction has the following characteristics (Figure 1):
- A premature P-wave occurs earlier than the sinus P-wave was expected.
- A premature P-wave has a different morphology (appearance), as compared with the sinus P-wave. The appearance depends on the location of the ectopic focus from which the impulse is discharged. If the impulse is discharged close to the sinoatrial node, the P-wave will be similar to the normal P-wave. If the impulse is discharged near the atrioventricular node, the atria will be depolarized in the opposite direction and thus generate a negative (retrograde) P-wave (Figure 2). Thus, the P-wave morphology of premature atrial beats is different from the sinus P-wave. Note that the P-wave might actually occur on the preceding T-wave if it is discharged very early.
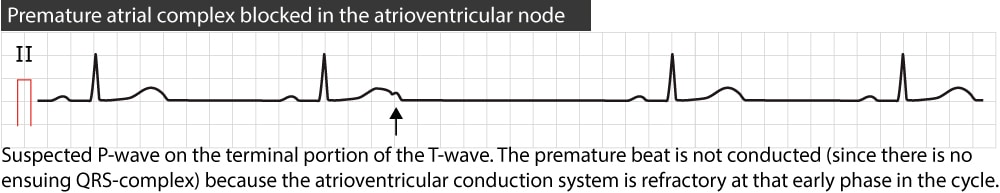
- The PR interval is normal in most cases but might be prolonged. Most premature atrial complexes are conducted through the atrioventricular node to the ventricles. The PR interval will typically be normal but it might be prolonged if the premature beat reaches the atrioventricular node before it has repolarized completely. The earlier the impulse reaches the atrioventricular node (and bundle of His), the longer the PR interval (because more fibers will be refractory). If the premature atrial impulse reaches the atrioventricular node (or bundle of His) while its completely refractory, the impulse will be blocked and no QRS complex appears.
The QRS complex appears if the atrial impulse is conducted to the ventricles. Because the impulse enters the ventricles through the bundle of His (which means that both bundle branches will conduct the impulse to each respective ventricle) the QRS complex is normal (i.e. QRS duration <0.12 s). However, the QRS complex can be wide (QRS duration ≥0.12 s) if there is a left or right bundle branch block. It is common that the premature atrial impulse arrives before one of the bundle branches has repolarized, which leads to a bundle branch block. This type of bundle branch block is termed aberration (or aberrant ventricular conduction), which was discussed previously. Figure 3 shows how a premature atrial contraction is conducted aberrantly.
Incomplete compensatory pause
A premature atrial contraction will most likely also depolarize the sinoatrial node and reset its clock. It will usually take some time for the impulse to travel from the ectopic focus to the sinoatrial node. Once the impulse has reset the sinoatrial node, the next sinus impulse will be discharged one normal sinus period from that time point. Hence, the interval between the premature beat and the next sinus beat will be equal to the time it takes for the impulse to travel to the sinoatrial node plus one sinus period. As evident in Figure 4, this means that the sinus beat after the premature beat will also occur earlier than expected (because the sinus node was discharged earlier than expected). The term incomplete compensatory pause implies that the interval between the sinus beats before and after the premature beat is less than two sinus periods (Figure 4).
A compensatory pause implies that the sinus beat after the premature beat occurs on schedule, such that there are two sinus cycles (2 RR intervals) between the beats before and after the premature beat. This is the hallmark of ventricular premature beats.
Variants of premature atrial contractions
Should the premature atrial impulse reach the atrioventricular node or bundle of His before these have repolarized sufficiently, the impulse will be blocked. Only the P-wave will appear on the ECG and it may be superimposed on the preceding T-wave (Figure 5).
Occasionally the premature atrial impulse affects the sinoatrial node such that it requires some additional time to recover. This prolongs the interval from the premature beat to the next sinus beat. The next sinus beat might actually occur where it would be expected (i.e. after a compensatory pause) or even later.
Similarly, if the premature atrial impulse fails to reset the sinoatrial node, the next sinus impulse will occur on schedule and activate the atria (if the atria have repolarized after the premature contraction). Hence, the premature atrial contraction will occur between two sinus beats (1 RR interval between the sinus beats), and this is referred to as an interpolated premature atrial beat.
If every other beat is an atrial premature contraction, it is called atrial bigeminy (Figure 6). If every third beat is an atrial premature contraction it is called atrial trigeminy. Similarly, there is quadrigeminy and so forth.
Clinical relevance
Premature atrial contractions are very common, both among healthy individuals and those with significant heart disease. The prevalence of premature atrial beats increases with age. It is considered normal to have a few premature atrial complexes per day. And the frequency increases during emotional stress, by drinking coffee and smoking. Premature atrial beats are more common among persons with heart disease, particularly conditions affecting the atria.
Note that if premature atrial beats are discharged frequently during rapid sinus rhythm or sinus tachycardia, it may resemble atrial fibrillation, which is why one should always look carefully for P-waves (which are not visible during atrial fibrillation).
Treatment of premature atrial contractions
Premature atrial contractions are only treated if the individual is symptomatic or if the beats precipitate tachyarrhythmias. Beta-blockers (usually bisoprolol tablets 5–10 mg once daily) or calcium channel blockers are the most effective alternatives.
Final note
A premature beat can also be referred to as an early beat, extrasystole, ectopic beat (because the impulse is discharged from an ectopic focus), or premature contraction. These terms are also used for premature impulses arising in the ventricles (discussed in the next article).