Pathological R-wave progression
Normal R-wave progression implies that the R-wave amplitude increases gradually from V1 to V5 and then diminishes again in V6. Refer to Figure 1. Abnormal R-wave progression implies that the gradual increase from V1 to V5 is absent. It may be broken, as in Figure 1. Any type of infarction may cause pathological R-wave progression. However, the specificity for pathological R-wave progression is considerably lower than pathological Q-waves and guidelines do not state any ECG criteria specific to R-wave progression.
U-wave changes
New U-waves (in absence of bradycardia) may indicate ischemia. If U-waves were present on previous recording, the amplitude must be increased in order to suggest ischemia. Inverted U-waves are even more typical of ischemia (but the sensitivity is low). U-wave changes always accompany other ischemic ST-T changes. They may occur in both NSTEMI and STEMI.
QTc prolongation
The QT (QTc) interval may be prolonged, shortened or unchanged in ischemia.
R-wave amplitude
Acute transmural ischemia may transiently increase the amplitude of the R-waves. This is believed to be due to delayed (and thus electrically unopposed) depolarization in the ischemic area.
Fragmented QRS complex
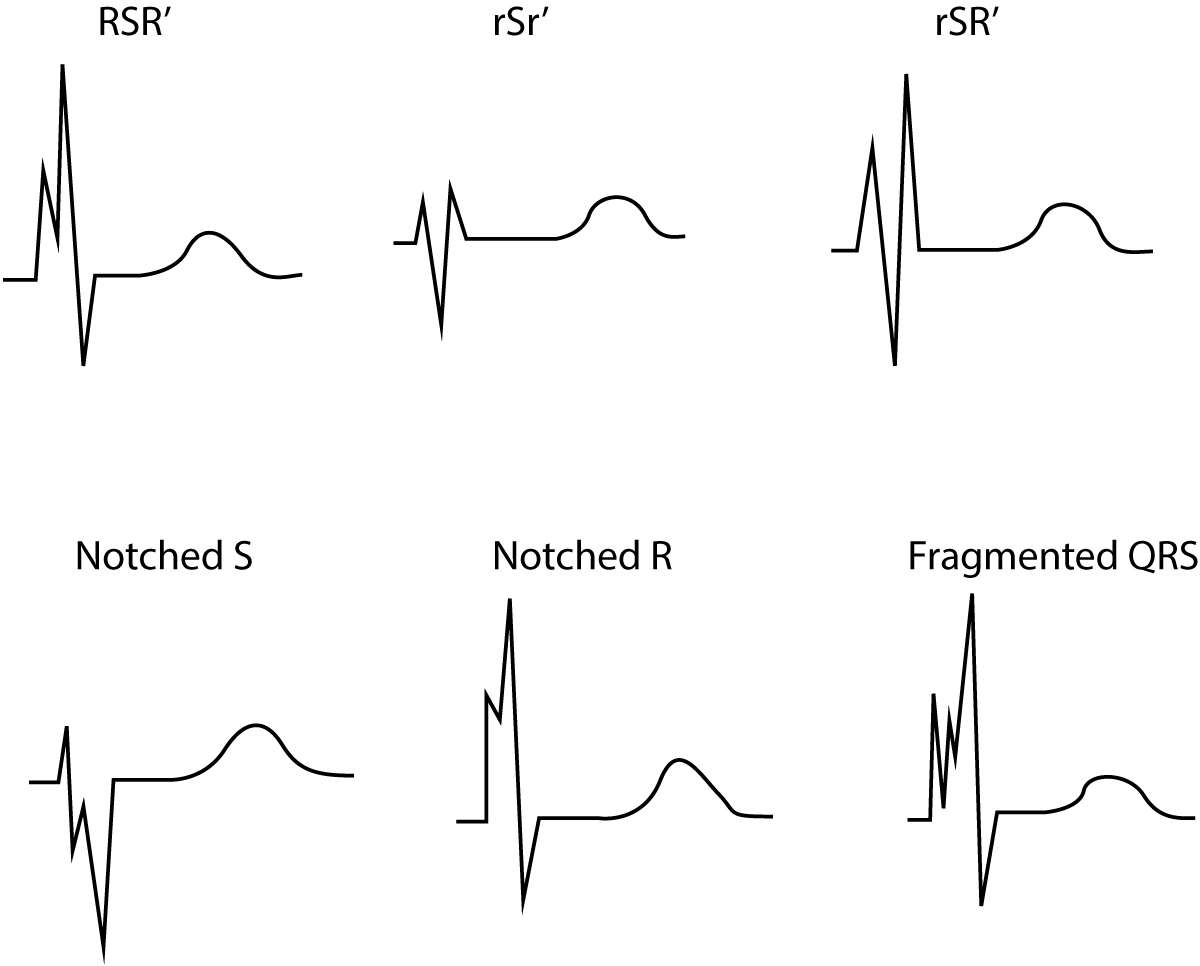
The definition of fragmented QRS complexes (Figure 2) are as follows:
- QRS complex with more than 1 R wave and/or
- notch in the descending limb of the R-wave and/or
- notch in the descending limb of the S-wave
In case of complete/incomplete bundle branch block or pacemaker rhythm, >2 notches are required in the S-wave or R-wave.