Principles of pediatric & neonatal ECG interpretation
Pediatric and neonatal ECG interpretation follow the same principles as ECG interpretation in adults, but there are important differences. These differences are largely explained by the dramatic physiological and anatomical changes that take place during infancy and childhood. The most dramatic changes occur during the first year of life. The electrocardiogram (ECG) evolves in parallel with the changing anatomy and physiology of the heart. ECG amplitudes, intervals and waveforms are therefore different in children and there are marked age variations throughout childhood. Clinicians who work in pediatric and neonatal care must have knowledge of age-related variations in the ECG, as well as cardiac diseases that may affect infants and children.
Physiological and anatomical development during infancy & childhood
In adults, the left ventricle is considerably larger than the right ventricle. This is the result of ventricular adaptation to the resistance that must be overcome by the ventricles. The left ventricle must overcome the pressure in the aorta and systemic circulation (normally 120 mmHg in adults). The right ventricle must overcome the pressure in the pulmonary circulation (normally 15 mmHg in adults). Hence, the pressure in the systemic circulation is many times greater than the pressure in the pulmonary circulation, which explains why the left ventricle is much larger (ventricular volume and muscle mass) than the right ventricle. Refer to Figure 1.
Figure 1. Cross-sectional view of ventricular wall thickness in children (<1 month old) and adults.
Because the left ventricle, in adults, is much larger than the right ventricle, the QRS complexes are dominated completely by the electrical currents generated by the left ventricle. This explains why leads V4–V6 normally displays large R-waves in adults (refer to The Normal ECG).
The fetal circulation
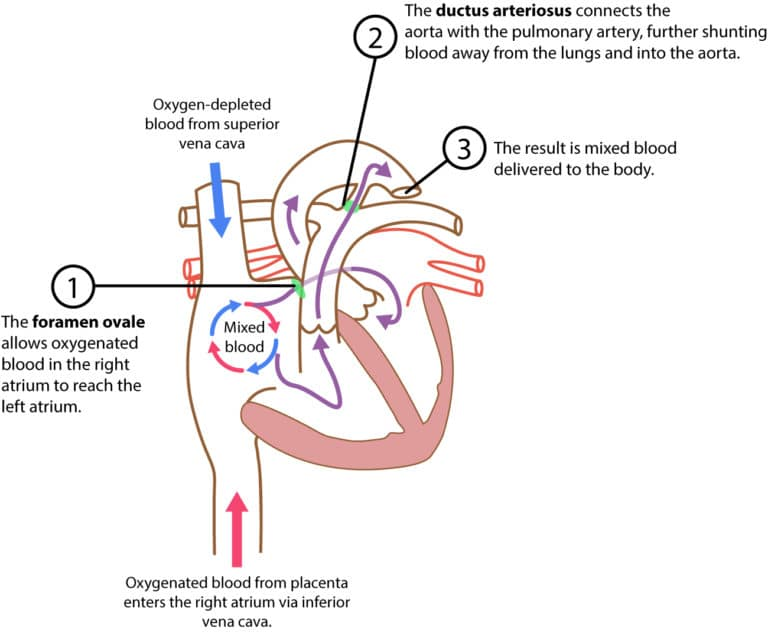
During the fetal period and the first month of life, the right ventricle is larger than the left ventricle. This is explained by the fact that the right ventricle pumps blood against greater resistance, as compared with the left ventricle. Understanding this requires knowledge of the fetal circulation, which is illustrated in Figure 2.
The fetus obtains oxygenated blood from the placenta via the inferior vena cava. Blood in the inferior vena cava continues to the right atrium. Meanwhile, deoxygenated blood in the superior vena cava (which returns blood from the head and upper limbs) also enters the right atrium. Oxygenated and deoxygenated blood is then mixed in the right atrium. In the fetus, there is an opening – namely the foramen ovale – between the right and left atrium. Most of the blood in the right atrium flows through the foramen ovale into the left atrium. The blood continues from the left atrium into the left ventricle, and from there it is pumped into the aorta (i.e systemic circulation. Note that blood also flows from the right atrium into the right ventricle, from where it is pumped into the pulmonary artery. In the fetus, a shunt called ductus arteriosus connects the pulmonary artery and the aorta. Since the resistance in the pulmonary circulation is high, the majority of the blood entering the pulmonary artery will be shunted through the ductus arteriosus into the aorta.
It is important to note that right ventricular load is greater than left ventricular load during the fetal period. This is explained by the configuration of the fetal circulation; pulmonary resistance is high (which means that resistance in the pulmonary artery is high), whereas resistance in the systemic circulation (and thus the aorta) is relatively low.
Figure 2. The fetal circulation. Adapted from Anatomy & Physiology OpenStax.
Therefore, the right ventricle is larger than the left ventricle during the fetal period. In the fetus, as well as in the newborn, the QRS complex is dominated by electrical currents generated by the right ventricle. Large R-waves in leads V1–V3 are therefore normal. Right ventricular dominance also explains why the electrical axis of the heart is more rightwards in newborns.
The postnatal circulation
The circulation undergoes dramatic changes after birth. The resistance (pressure) in the pulmonary circulation decreases immediately when the child takes her first breath and thereby right ventricular load drops rapidly. The ductus arteriosus closes, which results in increased perfusion in the pulmonary circulation.
Resistance in the systemic circulation increases, which results in increased left ventricular load. At the age of 1 month, the left ventricle is larger than the right ventricle. At the age of 6 months, the proportions (between right and left ventricles) are comparable to those seen in adults.
- Functional closure of the foramen ovale usually takes a few minutes to 24 hours. Anatomical closure occurs later. Right atrial pressure may vary during the first days after birth, which may explain shunting of blood through the foramen ovale during the first days.
- Ductus arteriosus closes completely within a few days after birth.
- Pulmonary resistance drops slowly, such that pressure in the right ventricle is at 25% of the left ventricle after 4 to 6 weeks.
As described above, the fetal circulation undergoes remarkable changes after birth. The process is, however, vulnerable. Any neonatal condition with hypoxia or acidosis may disrupt the adaptation process. Hypoxia and acidosis prevent vasodilatation in the pulmonary circulation. This results in persistent pulmonary hypertension, which may cause continued shunting of blood through the foramen ovale (from the right atrium to the left atrium). Because such shunting implies bypassing the lungs, cyanosis will ensue.
ECG intervals are proportional to myocardial mass
Because the child’s heart is small, compared with adults, it has fewer myocardial cells to depolarize and repolarize. This explains why all ECG intervals (PR interval, QRS duration, QTc interval, etc) are significantly shorter in children. As the heart grows, these intervals also increase.
Figure 3 presents an ECG recorded in an 8 days old female. The electrical axis deviates rightwards (negative QRS in lead I and positive QRS in lead II). R-waves are prominent in leads V1, V2 and V3. There are negative T-waves in V1–V3, which are also normal. There are Q-waves in inferior limb leads (II, aVF and III) and lateral chest leads (V5, V6).
Figure 3. ECG recorded in an 8 days old female. The electrical axis deviates rightwards (negative QRS in lead I and positive QRS in lead II). The R-waves are prominent in leads V1, V2 and V3. There are negative T-waves in V1–V3, which are also normal. There are Q-waves in inferior limb leads (II, aVF and III) and lateral chest leads (V5, V6).
Normal values (reference values) for ECG in neonatal and pediatric patients
There are numerous databases and publications on normal values in adults. However, there are few studies in the pediatric population. This is unfortunate since reference values play a central role in pediatric ECG interpretation. Clinicians have traditionally used normal values published in 1979 (Davignon et al) and in 2001 (Rijnbeek et al). The European Society for Cardiology recommends that normal values published by Davignon et al should be used for neonatal ECG interpretation, since Rijnbeek et al included too few children younger than 30 days. For children aged 30 days or older, both Rijnbeek et al and Davignon et al can be used. The difference between these two is, however, small and both are provided in detail below (refer to Normal values for pediatric and neonatal ECG interpretation).
Indications for ECG in children (neonatal and pediatric patients)
- Syncope
- Seizers
- Cardiopulmonary symptoms during exercise
- Poor physical performance
- Drug side effect or intoxication
- Tachycardia (tachyarrhythmia)
- Bradycardia (bradyarrhythmia)
- Cyanosis
- Heart failure
- Hypothermia
- Electrolyte imbalance
- Kawasaki disease
- Rheumatic heart disease
- Myocarditis, pericarditis, perimyocarditis
- Cardiac concussion
- Congenital heart disease
- Monitoring of vital parameters
- Post-operative monitoring