Atrial rhythms: ectopic atrial rhythm, atrial tachycardia and multifocal atrial tachycardia
Ectopic atrial tachycardia (or simply atrial tachycardia) occur when an ectopic focus in one of the atria discharges impulses at a higher rate than the sinoatrial node. This is due to abnormal automaticity or re-entry (triggered activity is much less common) taking place in the ectopic focus. The atrial rate ranges from 120 to 250 beats per minute. Note that the ventricular rate must exceed 100 beats per minute for it to be classified as ectopic atrial tachycardia. If the ventricular rate is lower, then it is classified as ectopic atrial rhythm.
Ectopic atrial tachycardia primarily affects individuals with heart disease but it occasionally occurs in otherwise healthy individuals. Presence of lung disease, use of theophyllamine, and catecholamines may induce atrial tachycardia. The tachycardia starts abruptly, although it sometimes has an initial warm-up period of 5 to 10 seconds. Atrial tachycardia is characterized by occurring in short and rapid bursts. In most cases it is self-terminating, but it may recur and in some cases persist for longer periods. As for any other long-standing tachycardia, there is a risk of developing tachycardia-induced cardiomyopathy.
Children may be affected by a special type of atrial tachycardia caused by embryological rests in the atria. These embryological remnants may have very high automaticity.
Note that the term “ectopic” is often dropped when referring to these arrhythmias.
The ECG in ectopic atrial rhythm and atrial tachycardia
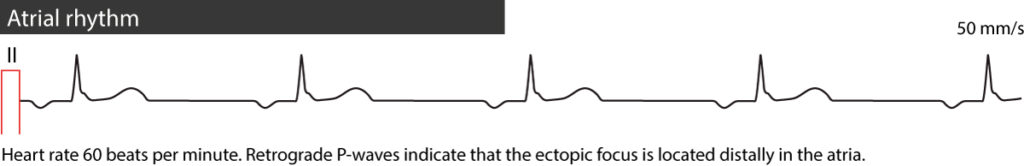
- A regular rhythm with P-waves that differ (in terms of contour/appearance) from the sinus P-waves. If the P-waves in lead II are retrograde (negative), the diagnosis is simple because sinus P-waves can never be negative in lead II. If the P-waves are positive in lead II, it is usually necessary to compare the P-wave contour during tachycardia with the P-waves during sinus rhythm.
- The isoelectric line (baseline) does not have a saw-tooth pattern, which it does during atrial flutter.
- All P-waves are followed by QRS complexes. AV block is unusual unless the patient is treated with digoxin.
- The ventricular rate is regular, ranging between 100 and 250 beats per minute in atrial tachycardia, and less than 100 beats per minute in atrial rhythm.
Refer to ECG examples in Figure 1, 2 and 3 below.
Figure 1. Atrial rhythm.
Figure 2. Atrial tachycardia.
Causes of ectopic atrial tachycardia and ectopic atrial rhythm
- Side effect of digoxin.
- Congestive heart failure.
- Lung disease (COPD, pulmonary hypertension, etc).
- Ischemic heart disease (coronary artery disease).
- Structural heart disease of any kind.
Treatment of atrial tachycardia
Stopping digoxin medication is sufficient in patients using the drug. Management of all other patients follows the management for atrial fibrillation and atrial flutter (refer to these articles). Beta-blockers, digoxin and calcium channel blockers may all be used to lower ventricular rate. If these interventions are inadequate, it is reasonable to try class IA, IC or III antiarrhythmic drugs. Ablation therapy should be considered if there is risk of recurrence. Note that electrical cardioversion should not be attempted because it is ineffective in treating atrial tachycardia.
Multifocal atrial tachycardia
Multifocal atrial tachycardia is an unusual variant of ectopic atrial tachycardia. As seen in Figure 4, it is characterized by an irregular rhythm with clearly visible P-waves (on the contrary to atrial fibrillation) but the P-wave morphology varies from one beat to another. This is explained by the fact that there are multiple ectopic foci that discharge impulses which lead to atrial activation. Multifocal atrial tachycardia starts gradually. In most cases there is 1:1 ventricular response, meaning all atrial impulses are conducted to the ventricles. The ventricular rate ranges between 100 and 150 beats per minute.
Multifocal atrial tachycardia may be intermittent with intervening periods of sinus rhythm. The most common underlying causes are heart failure, atrial ischemia, increased atrial pressure, use of theophyllamine or chronic lung disease (particularly chronic obstructive pulmonary disease). Multifocal atrial tachycardia may occur in children.
Note that if the atrial rhythm is below 100 beats per minute, it is referred to as multifocal atrial rhythm.
Treatment of multifocal atrial tachycardia
Treatment should be targeted at the underlying cause. This usually resolves the arrhythmia. Electrical cardioversion is contraindicated as it may worsen the arrhythmia. Beta-blockers should be considered as first choice (provided that pulmonary disease does not limit its use). Antiarrhythmic drugs have unsatisfactory effects. Diltiazem, verapamil and amiodarone may be considered. Additionally, magnesium and potassium substitution should also be considered.